Glycine Injection
This product is available solely through our 503B Outsourcing Facility, offering you the highest standards of quality and safety in every purchase. If you do not have an account, please contact us.
Product Overview
Glycine Injection is a compounded sterile solution of the amino acid glycine. Glycine is the simplest naturally occurring amino acid and is classified as nonessential in humans (meaning the body may synthesize it endogenously).[1]
Despite being “nonessential,” glycine plays critical roles in normal physiology. It is a fundamental building block of proteins and is involved in the synthesis of DNA, glutathione, creatine, and other important biomolecules.
Clinically, glycine has been used as a component of total parenteral nutrition and has been investigated in various therapeutic contexts. For example, it has been studied as an adjunctive treatment in certain neurological conditions (such as schizophrenia) due to its activity in the central nervous system.[2] It has also been utilized historically in diagnostic provocation tests (e.g., to stimulate growth hormone release) and as an irrigating fluid in surgical settings (in much more dilute form).
As a compounded medication dispensed by a 503B outsourcing facility, Glycine injection is prepared for office use. All potential uses of this injection should be supported by careful consideration of the patient’s condition and current scientific evidence.
The therapeutic benefits of supplemental glycine remain an area of ongoing research, and robust clinical efficacy data are limited. Providers typically reserve glycine injection for specialized needs – for instance, as part of a tailored amino acid supplementation regimen – and treatment should only be initiated and monitored by qualified healthcare professionals in accordance with applicable laws and guidelines.[4]
Disclaimer: This compounded medication is prepared under section 503B of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
Glycine’s mechanism of action in the body is multifaceted, reflecting its diverse roles as both a neurotransmitter and a metabolic substrate.
In the central nervous system, glycine functions as a neurotransmitter with dual properties. It is one of the major inhibitory neurotransmitters in the spinal cord and brainstem, akin to gamma-aminobutyric acid (GABA). When glycine binds to inhibitory glycine receptors (which are chloride channel complexes), it causes an influx of chloride ions into neurons, hyperpolarizing the cell membrane and thereby reducing neuronal excitability.[1] This inhibitory action contributes to glycine’s calming and reflex-modulating effects on the spinal cord – for example, helping regulate motor neuron activity and muscle tone.
At the same time, glycine is also an obligatory co-agonist at N-methyl-D-aspartate (NMDA) receptors, a type of excitatory glutamate receptor in the brain. Glycine must occupy its modulatory binding site on the NMDA receptor complex for glutamatergic neurotransmission to fully occur. Through this role, glycine positively modulates NMDA receptor activity, which is involved in processes such as synaptic plasticity, learning, and memory. (Notably, this NMDA co-agonist function underlies research into glycine for neuropsychiatric conditions; by enhancing NMDA receptor function, high-dose glycine has been reported to influence symptoms in schizophrenia in some studies.)[2][5][6]
Peripherally, glycine serves as a key building block and metabolic molecule. It is integral to collagen structure – approximately one-third of the amino acid content of collagen (the main connective-tissue protein) is glycine. Every third residue in the collagen triple helix is a glycine molecule, a fact that highlights glycine’s importance in maintaining the tensile strength and integrity of skin, bones, cartilage, and tendons.[3]
Glycine is also a precursor for several critical biomolecules. It contributes to the synthesis of creatine (essential for muscle energy storage), porphyrins such as heme (the oxygen-carrying component of hemoglobin), purines (components of DNA and RNA), and it conjugates with bile acids to form bile salts (facilitating fat digestion). In addition, glycine combines glutamate and cysteine to form glutathione, the body’s primary intracellular antioxidant. By influencing glutathione availability, glycine may affect oxidative stress and detoxification pathways in cells.
Given these roles, an administered dose of glycine (such as 50 mg/mL injection) may have both neuromodulatory and metabolic effects. For instance, increasing plasma glycine through injections may transiently augment inhibitory neurotransmission (potentially producing a mild sedative or muscle-relaxant effect) and support anabolic processes like collagen deposition or antioxidant synthesis.
The net physiological effect of Glycine Injection may depend on the dose and route of administration: lower doses may primarily supplement normal metabolic needs, while high doses (especially if given rapidly) may cross the blood-brain barrier and significantly alter neurotransmitter dynamics.[2]
Overall, the mechanism of glycine’s action is complex, spanning from central nervous system neurotransmission to peripheral tissue biosynthesis, which underscores why glycine has been explored in contexts ranging from neurological disorders to wound healing.
Because glycine is an amino acid naturally present in the body, there are relatively few absolute contraindications to its use; however, certain conditions preclude or caution against Glycine Injection (50 mg/mL) due to the risk of adverse outcomes.
Severe renal impairment, especially anuria (inability to produce urine), is a primary contraindication. Patients who are anuric or have substantially compromised kidney function should not receive glycine injections because they cannot adequately excrete the glycine load and excess fluid. In such cases, administration could lead to fluid overload or accumulation of metabolic byproducts.
Similarly, severe heart failure or pulmonary edema represents a contraindication or strong precaution for glycine administration. Large amounts of glycine solution, if absorbed systemically, may expand intravascular volume and precipitate or worsen congestive heart failure or pulmonary congestion; thus, patients with poor cardiopulmonary reserve should generally not be exposed to significant glycine infusions.[7][8]
Hepatic impairment is another important consideration. Glycine is mainly metabolized via the liver (one pathway converts glycine to serine, with the concomitant production of ammonia). In patients with severe liver dysfunction, the normal metabolism of glycine may be impaired, risking accumulation of ammonia and possible hyperammonemia. Therefore, glycine injection should be avoided or used only with great caution in those with advanced liver disease or disorders of ammonia metabolism.
Additionally, although true allergies to glycine are exceedingly rare (glycine is a ubiquitous natural molecule), any prior hypersensitivity reaction to glycine or to components of the formulation would contraindicate its use. The glycine injection contains glycine in sterile water (and possibly a pH buffer); documented allergies to any of these would preclude administration.
Patients with the rare metabolic disorder non-ketotic hyperglycinemia (a congenital glycine encephalopathy) would also be contraindicated from receiving glycine, since they already have toxic elevated glycine levels in the CNS and additional glycine could worsen their condition.
In summary, Glycine Injection should not be used in patients who cannot properly metabolize or excrete amino acid or the solution load. All candidates for therapy require a thorough medical evaluation. The prescribing practitioner must screen for conditions like renal failure, hepatic insufficiency, or cardiopulmonary compromise, and should only proceed with glycine supplementation if the potential benefits outweigh the risks in these contexts. Close monitoring is advised whenever glycine is administered to anyone with borderline organ function.
Glycine is an amino acid and not a classic enzyme-inhibiting drug, but it may still interact with other medications through pharmacodynamic and physiologic mechanisms.
One well-documented interaction is with the atypical antipsychotic clozapine. High-dose glycine supplementation has been reported to interfere with clozapine’s therapeutic efficacy in schizophrenia patients.[1] In a clinical study, schizophrenia patients on clozapine who received adjunctive glycine did not experience the usual improvement in symptoms – in fact, glycine co-administration appeared to diminish clozapine’s antipsychotic effects.
The likely basis of this interaction is at the level of glutamatergic neurotransmission: clozapine is thought to modulate NMDA receptor function (possibly by influencing the glycine-binding site), so extra glycine may alter this balance, leading to reduced drug efficacy.[1] Due to this, patients being treated with clozapine are generally advised not to take glycine (in any form) unless under close psychiatric supervision. If a clinician does consider glycine for a patient on clozapine, careful monitoring of psychiatric status is essential, and discontinuing glycine should be the first step if any deterioration in symptom control is observed.[9][10]
Beyond clozapine, glycine’s interactions largely stem from its role as an inhibitory neurotransmitter. CNS depressants may have additive effects with glycine. For example, concurrent use of glycine injection with sedative-hypnotic medications (such as benzodiazepines, barbiturates, or opioid analgesics) could potentially enhance sedation or respiratory depression.
While no formal drug-drug interaction studies have been conducted for glycine in this context, this caution is based on the understanding of glycine’s inhibitory action in the brainstem and spinal cord (which might synergize with other depressants to further reduce neural activity). Thus, healthcare providers should exercise caution when administering glycine to patients on other sedating drugs, and patients should be observed for excessive drowsiness or slowed breathing.
Glycine may also interact with substances that affect amino acid metabolism. For instance, valproic acid (an anticonvulsant) is known to raise ammonia levels by affecting hepatic amino acid processing; adding glycine (which is metabolized to ammonia and CO2) could in theory exacerbate ammonia accumulation. Patients on valproate or with urea cycle disorders should therefore use glycine carefully, if at all, with ammonia levels monitored as needed.
Finally, it’s worth noting that glycine may chelate certain minerals in solution (it’s sometimes used in mineral supplements as a chelating agent), but in vivo this is not a significant issue at the doses given by injection.
In summary, while glycine does not have extensive drug interactions, its concurrent use with neuroactive drugs requires prudence. Always inform your healthcare provider of all the medications and supplements patients are taking before starting glycine injection, so that potential interactions may be anticipated and managed safely.
Because glycine is a substance the body ordinarily uses and metabolizes, low-dose glycine injections are generally well tolerated. Many patients may not experience any noticeable side effects at modest doses. However, glycine in pharmacologic doses (or rapid infusions) may produce a range of adverse reactions. The side effect profile may be understood by considering glycine’s pharmacologic actions and the effects of the solution’s administration.
At relatively low doses, mild sedation or drowsiness is one of the reported side effects of glycine supplementation.[1] Glycine’s inhibitory neurotransmitter function in the CNS may induce a calming effect; a small number of individuals have noted feeling slightly lethargic or lightheaded after glycine injection. This sedative-like effect is usually transient and not severe, often manifesting as a sense of relaxation or slight dizziness. Along with this, nausea is another possible side effect, especially if glycine is infused rapidly or in large amounts. Some patients have reported stomach discomfort, including nausea or even vomiting, following high-dose glycine administration. Glycine’s taste (in oral form) is sweet, but intravenously it may sometimes cause an odd sensation or mild GI upset as the body adjusts to the amino acid load.
Glycine Injection, being a solution, also carries risks related to the volume and osmolarity of fluid administered. Rapid or excessive volumes of glycine 50 mg/mL may lead to fluid and electrolyte disturbances. For instance, large intravenous infusions have, in surgical contexts, resulted in dilutional hyponatremia (low sodium levels) and fluid overload. Patients absorbing very large volumes of glycine (as was noted in historical case reports during prostate or uterine surgery irrigations) developed symptoms like confusion, nausea, high blood pressure, or low blood pressure as a result of these imbalances. In extreme cases, hyperglycinemia (excessively high plasma glycine levels) may occur if injection doses are very large or elimination is impaired. This may overwhelm normal metabolic pathways, leading to elevated ammonia in the bloodstream (since glycine catabolism produces ammonia). Consequences of acute hyperammonemia and hyperglycinemia may include neurologic symptoms such as headache, disorientation, encephalopathy, seizures, or even coma in severe scenarios. It must be emphasized that such severe outcomes are exceedingly rare in the context of typical dosing; they have been observed primarily in cases of accidental glycine overexposure (for example, absorption of many liters of glycine irrigant during a surgical procedure) rather than a single 30 mL vial injection. Nonetheless, these possibilities underscore the importance of proper dosing and monitoring.
Other side effects documented with glycine use include: lightheadedness or a feeling of faintness (likely related to mild hypotension or CNS effects), increased salivation (anecdotally noted with high IV doses), and in rare instances, visual disturbances. Transient blurred vision or temporary visual field changes (such as a brief dimming of vision) have been reported when large amounts of glycine were rapidly introduced into the bloodstream. This is thought to result from glycine’s action on retinal neurotransmitter receptors (the retina also contains inhibitory glycine receptors, and glycine toxicity may affect vision). These visual side effects reverse as glycine levels normalize.
Importantly, allergic reactions to glycine are exceedingly rare or essentially unheard of in medical literature. Glycine is a natural amino acid present in all proteins, so the immune system typically recognizes it as a “self” molecule. There have been no significant reports of anaphylaxis purely to glycine. However, any injection may trigger injection-site reactions or sensitivity to additives. If a patient experiences rash, itching, or breathing difficulty after glycine injection, medical attention should be sought, even though glycine itself is an unlikely culprit.
In clinical use, most side effects of glycine may be mitigated by controlling the infusion rate and total dose. Administering the injection slowly allows the body to metabolize and distribute the amino acid without acute spikes in concentration. Healthcare providers may monitor vital signs (such as blood pressure, heart rate, and neurological status) during and after administration, especially for higher doses, to may help ensure patient safety.
Overall, glycine’s safety profile is favorable at the doses typically used, with sedation and mild nausea being the most commonly noted effects.[1] Serious adverse outcomes are avoidable by adhering to recommended dosing parameters and precautions. Any unusual or severe symptoms following glycine injection should be promptly evaluated, and the infusion stopped if necessary.
The use of Glycine Injection during pregnancy requires careful consideration, as safety data are very limited. Glycine is a naturally occurring amino acid that plays a role in fetal development (it is required for fetal protein and collagen synthesis), but the administration of high-dose glycine to pregnant women has not been well studied. No animal reproductive studies or controlled human studies have been conducted to evaluate potential teratogenic or toxic effects of glycine supplementation in pregnancy. It is therefore unknown whether glycine injection could cause fetal harm or affect reproductive capacity. According to available drug labeling and guidelines, glycine injections should be given to a pregnant woman only if clearly needed – in other words, only if the potential benefit to the mother outweighs any possible risk to the fetus.[1] This cautious approach is standard for medications without robust safety data in pregnancy.[11][12]
It is important to distinguish between dietary glycine and pharmacologic glycine dosing. Pregnant individuals obtain glycine through normal protein intake, and glycine is naturally present in the maternal circulation. In fact, emerging research indicates that glycine demand increases in later stages of pregnancy – glycine may become “conditionally indispensable” (conditionally essential) in the third trimester, meaning that dietary intake of glycine (or its precursors) is critical as endogenous synthesis may not meet fetal needs. One study found that late-gestation pregnant women have a higher metabolic requirement for glycine, presumably for fetal growth and collagen formation.[3] However, this increased physiological need does not imply that direct glycine injections are recommended; rather, it underscores the importance of adequate protein nutrition. Until more research is available, glycine 50 mg/mL injections are generally avoided during pregnancy unless no viable alternative exists. For example, if a pregnant patient had a specific severe amino acid deficiency or clinical condition that a physician determines could be helped by glycine, and no other treatment is appropriate, only then might glycine injection be considered, with informed consent and close monitoring.
When glycine injection (or any amino acid therapy) is used in a pregnant woman, the healthcare team may monitor both mother and fetus closely. Parameters such as maternal ammonia levels (since excessive glycine could raise ammonia) and ultrasound assessments of fetal well-being might be checked if the exposure is ongoing. Thus far, there have been no reports linking glycine supplementation to birth defects or pregnancy loss, but the absence of data means uncertainty.
Breastfeeding considerations are similar: glycine is a normal component of breast milk, but the effects of extra glycine on a nursing infant are unknown. It would be expected that a mother’s body would regulate excess glycine, and only small amounts would appear in milk, but caution dictates using glycine therapy only if necessary during lactation as well.[2]
In summary, glycine should be treated like any supplement in pregnancy – with caution. The official recommendation is that glycine not be used by pregnant or breastfeeding women unless the potential benefits justify the potential risks.[1] Women who are pregnant, planning to become pregnant, or nursing should discuss all supplements and compounded medications with their healthcare provider. The provider may likely choose to err on the side of caution, reserving glycine injection for situations of clear medical need.
Proper storage of Glycine Injection is important to maintain its stability and sterility. This compounded injection should be stored at controlled room temperature, generally around 20°C to 25°C (68°F to 77°F). It is advisable to keep the vial in a cool, dry place, protected from excessive heat and direct light. Do not freeze the vial. Freezing an aqueous amino acid solution could cause precipitation or container damage.[15]
Glycine Injection vials should remain in their original packaging until use. The vial’s rubber stopper and seal help maintain sterility; once punctured or opened, the contents should be used promptly or within the timeframe specified on the label.
Before administering glycine, inspect the solution visually. The liquid should be clear and free of particulate matter. Do not use the injection if you notice cloudiness, discoloration, or any particles floating in the solution. Such changes could indicate contamination or degradation. If the vial was accidentally frozen and then thawed, or if it was stored improperly, these issues might occur.
- Heresco-Levy, U., Javitt, D. C., Ermilov, M., Mordel, C., Silipo, G., & Lichtenstein, M. (1999). Efficacy of high-dose glycine in the treatment of enduring negative symptoms of schizophrenia. Archives of General Psychiatry, 56(1), 29–36. https://doi.org/10.1001/archpsyc.56.1.29
- Sheffler, Z. M., Reddy, V., & Pillarisetty, L. S. (2021). Physiology, Neurotransmitters. In StatPearls [Internet]. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539894/
- Reiche, L. (2020). Collagen. DermNet NZ. Retrieved from https://dermnetnz.org/topics/collagen
- Drugs..com. (2025). Glycine: Package insert / prescribing information. Drugs.com. https://www.drugs.com/pro/glycine.html
- Zafra, F., Aragón, C., & Giménez, C. (1997). Molecular biology of glycinergic neurotransmission. Molecular Neurobiology, 14(3), 117–142. https://doi.org/10.1007/BF02740653
- Salceda, R. (2022). Glycine neurotransmission: Its role in development. Frontiers in Neuroscience, 16, 947563. https://doi.org/10.3389/fnins.2022.947563
- WebMD. (2023). Glycine: Uses and risks. WebMD. https://www.webmd.com/vitamins-and-supplements/glycine-uses-and-risks
- Truemeds. (2024). Glycine drug information. Truemeds. https://www.truemeds.in/drug-salts/glycine-5632
- Potkin, S. G., Jin, Y., Bunney, B. G., Costa, J., & Gulasekaram, B. (1999). Effect of clozapine and adjunctive high‑dose glycine in treatment‑resistant schizophrenia. American Journal of Psychiatry, 156(1), 145‑147. https://doi.org/10.1176/ajp.156.1.145
- Schwieler, L., Linderholm, K. R., Nilsson‑Todd, L. K., Erhardt, S., & Engberg, G. (2008). Clozapine interacts with the glycine site of the NMDA receptor: Electrophysiological studies of dopamine neurons in the rat ventral tegmental area. Life Sciences, 83(5–6), 170‑175. https://doi.org/10.1016/j.lfs.2008.05.014
- Barrow, P., Parrott, N., Alberati, D., Paehler, A., & Koerner, A. (2016). Preclinical reproductive and developmental toxicity profile of a glycine transporter type 1 inhibitor, bitopertin. Birth Defects Research Part B: Developmental and Reproductive Toxicology, 107(3), 180‑189. https://doi.org/10.1002/bdrb.21179
- Bumrungpert, A., et al. (2022). Efficacy and safety of ferrous bisglycinate and folinic acid in the control of iron deficiency in pregnant women: A randomized, controlled trial. Nutrients, 14(3), 452. https://doi.org/10.3390/nu14030452
- WebMD. (2024). Glycine: Uses, side effects, and more. WebMD. https://www.webmd.com/vitamins/ai/ingredientmono-1072/glycine
- U.S. Food and Drug Administration. (2019). 1.5% Glycine irrigation, USP prescribing information [Package insert]. FDA. https://www.fda.gov/media/108909/download
- U.S. Food and Drug Administration. (1998). Glycine irrigation solution—label information [Drug label]. FDA. https://www.accessdata.fda.gov/drugsatfda_docs/label/1998/20849lbl.pdf
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.
We're licensed to ship nationwide.
We ship orders directly to you, quickly and discreetly.


 Arginine HCl Injection
Arginine HCl Injection Taurine Injection
Taurine Injection Bi-Amino Injection
Bi-Amino Injection Lysine HCL Injection
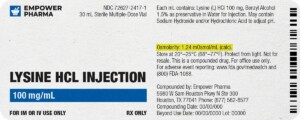
Lysine HCL Injection Glutathione Injection
Glutathione Injection