Tirzepatide / Niacinamide Injection
This product is available solely through our 503A Compounding Pharmacy, ensuring personalized care and precision in every order. Please note that a valid prescription is required for purchase. If you do not have an account, please contact us.
Product Overview
Tirzepatide/Niacinamide Injection is a compounded subcutaneous medication that combines tirzepatide, a novel dual incretin mimetic, with niacinamide (vitamin B3). Tirzepatide is a glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved for adults with type 2 diabetes mellitus to improve glycemic control and obseity.[1] By activating both GIP and GLP-1 pathways, tirzepatide may enhance insulin secretion and decrease glucagon release in the presence of elevated blood glucose, helping to lower blood sugar levels.[1]
Niacinamide, also known as nicotinamide, is a form of vitamin B3 included in this formulation as a supportive ingredient. Niacinamide is water-soluble and plays a crucial role in the body’s metabolic processes. It serves as a precursor to the coenzymes NAD and NADP, which are required by hundreds of enzymes involved in energy production and cellular function.[4] Adequate vitamin B3 levels may support healthy digestion, nerve function, and skin maintenance, and are essential for converting food into energy.[5] In this injection, niacinamide is intended to potentially enhance metabolic support and stability of the formulation. Preliminary research even suggests that nicotinamide supplementation may influence body weight and fat metabolism: in an animal study, niacinamide protected against diet-induced weight gain, increased energy expenditure, and promoted the browning of white fat tissue.[6] While such effects in humans are unproven, the inclusion of niacinamide is generally regarded as being potentially beneficial for overall metabolic health. Importantly, the niacinamide dose in this combination is modest (2 mg/mL), so it may primarily act as a vitamin co-factor without the high doses of niacin that are associated with flushing or cholesterol-lowering pharmacotherapy.
This compounded injection is available in multiple strengths for tailored dosing. Tirzepatide/Niacinamide Injection is provided at 17 mg/2 mg per mL (tirzepatide/niacinamide) in 4 mL and 2 mL vials, as well as 8 mg/2 mg per mL in a 2.5 mL vial. Therapy with tirzepatide is typically initiated at a low dose and titrated gradually based on clinical response and tolerability. Like other GLP-1 receptor agonist therapies, tirzepatide is administered as a once-weekly subcutaneous injection.[1] The combination with niacinamide does not change the dosing schedule. Patients should use this medication only with a valid prescription and under healthcare provider guidance, as part of a comprehensive plan for managing diabetes and/or weight. The following sections detail the injection’s mechanism of action, precautions, and proper usage.
Tirzepatide’s mechanism of action is distinctive in that it agonizes two incretin receptors simultaneously. As a “twincretin,” tirzepatide mimics the actions of endogenous GIP and GLP-1 hormones.[1] Upon subcutaneous administration, it binds to GIP and GLP-1 receptors in pancreatic islet cells and other tissues. This dual receptor activation leads to glucose-dependent insulin secretion from pancreatic β-cells and suppression of glucagon secretion from α-cells when blood glucose is elevated.[1] By enhancing insulin release (only when needed for high glucose) and reducing excess glucagon, tirzepatide helps reduce fasting and postprandial blood glucose levels. In addition, activation of GLP-1 receptors in the brain and gastrointestinal tract slows gastric emptying and promotes satiety, thereby reducing appetite and caloric intake.[1] Patients often experience a feeling of fullness and decreased appetite, which contributes to weight loss over time.
Through these mechanisms, tirzepatide achieves greater metabolic effects than single-pathway therapies. Its dual agonism has been associated with stronger glycemic control and weight reduction compared to traditional GLP-1–only agonists.[1] For example, tirzepatide has been shown to significantly improve markers of insulin sensitivity and beta-cell function, reflecting its comprehensive action on metabolic pathways.[3] The weight loss effect is largely attributed to decreased appetite and caloric intake, but tirzepatide may also modestly increase energy expenditure by raising adiponectin levels and altering fat utilization.[1] Meanwhile, niacinamide’s mechanism in this combination is as a vitamin co-factor. Niacinamide is incorporated into NAD/NADP, facilitating numerous oxidation-reduction reactions in metabolism.[4] Sufficient niacinamide ensures that cells can efficiently convert nutrients into ATP, supporting the energy demands of tissues. While niacinamide itself does not directly lower glucose, it may assist overall metabolic function and cellular health.
Tirzepatide/niacinamide injection should be used with caution and is contraindicated in certain patients. Because tirzepatide belongs to the GLP-1 receptor agonist class, it carries a boxed warning (from animal data) regarding thyroid C-cell tumors. Patients with a personal or family history of medullary thyroid carcinoma (MTC) or those with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2) must not use tirzepatide.[1] In rodent studies, chronic tirzepatide exposure caused thyroid C-cell tumors; although the relevance to humans is not confirmed, an abundance of caution is warranted. Any patient with a history of MTC or MEN2 is contraindicated due to this theoretical cancer risk. Additionally, tirzepatide is contraindicated in patients who have had a serious hypersensitivity reaction to tirzepatide or any of the formulation components (e.g. anaphylaxis or angioedema).[1] If a patient has known severe allergies to similar GLP-1 agonist medications, this injection should generally be avoided to prevent the risk of a life-threatening reaction.
There are also important precautions and relative contraindications to consider. Tirzepatide is approved only for type 2 diabetes and has not been studied in patients with type 1 diabetes mellitus or diabetic ketoacidosis; it should not be used as a substitute for insulin in those conditions.[1] Patients with gastroparesis or severe gastrointestinal disorders should use tirzepatide cautiously, as it delays gastric emptying and could worsen GI symptoms. A history of pancreatitis is another concern – tirzepatide has not been studied in patients with pancreatitis, and GLP-1/GIP agonists have been associated with rare cases of pancreatitis. Providers may decide to avoid tirzepatide in individuals with a history of pancreatitis or gallbladder disease, since rapid weight loss can predispose to gallstones. Diabetic retinopathy is another consideration: rapid improvements in blood sugar (as can occur with effective therapy) may transiently worsen diabetic eye disease. Patients with retinopathy should be monitored closely, though this is a precaution rather than an absolute contraindication. In summary, tirzepatide/niacinamide injection is contraindicated for patients with MTC/MEN2 or known tirzepatide allergy, and it is not indicated for type 1 diabetes. Caution is advised in those with a history of pancreatitis, severe GI conditions, gallbladder disease, or diabetic eye complications. All patients should be evaluated by a healthcare professional to ensure the therapy is appropriate for their individual medical history.
Tirzepatide has a relatively low potential for pharmacokinetic drug-drug interactions because it is a peptide that is metabolized to amino acids and does not strongly induce or inhibit cytochrome P450 enzymes.[1] However, its physiological effects can impact other medications, particularly oral drugs. The most notable interaction is due to delayed gastric emptying caused by tirzepatide. By slowing the rate at which the stomach empties, tirzepatide may reduce the absorption speed of oral medications taken around the same time. Although with continued weekly use this effect diminishes (gastric emptying delay is most pronounced after the first dose), clinicians should be aware that tirzepatide may transiently decrease the effectiveness of oral medications, especially those that require consistent absorption.[1]
Oral contraceptives deserve special mention: women on birth control pills are advised to use an alternative or backup contraceptive method when starting tirzepatide or increasing the dose, to avoid unintended pregnancy.[1] In practice, a barrier method or non-oral contraceptive should be used for at least 4 weeks after initiation or dose escalation of tirzepatide, due to the potential reduction in oral contraceptive absorption. Aside from affecting oral drug absorption, tirzepatide’s dual incretin action can interact pharmacodynamically with other diabetes medications. Concomitant use with insulin or sulfonylureas can increase the risk of hypoglycemia (because tirzepatide and these agents all lower blood glucose). If tirzepatide is added to a patient already on insulin or a sulfonylurea, the doses of those agents may need to be reduced and blood sugars monitored closely to prevent low blood sugar episodes. Tirzepatide should also not be used alongside other GLP-1 receptor agonists (e.g., semaglutide or liraglutide) since the combination has not been studied and could increase side effects without additional benefit.[1]
In summary, tirzepatide/niacinamide injection may interact with medications by slowing gastric emptying and enhancing hypoglycemic effects. Patients should inform their healthcare provider of all medications and supplements they are taking. Important points include using caution with oral drugs (especially birth control pills and narrow therapeutic index drugs) and adjusting doses of insulin or insulin secretagogues to mitigate hypoglycemia. By managing the timing of oral medications and monitoring glucose closely, most drug interactions with tirzepatide can be navigated safely.
Adverse effects with tirzepatide/niacinamide injection are generally similar to those observed with GLP-1 receptor agonists, with gastrointestinal symptoms being the most common. Overall, most patients tolerate tirzepatide well, and side effects, if they occur, are often mild to moderate and dose-dependent⁷. The primary side effects are related to the gut: nausea, decreased appetite, and indigestion are frequently reported, especially during the initial weeks of therapy. Diarrhea is also relatively common, and a smaller percentage of patients may have vomiting episodes, particularly as doses are escalated.[7] These GI symptoms are usually transient and improve as the body adjusts; using a gradual dose titration (starting low and increasing slowly) helps minimize these effects. Some patients also report constipation or bloating, though less frequently than nausea or diarrhea. Because tirzepatide delays gastric emptying, it can cause a feeling of fullness—this contributes to its therapeutic effect on appetite, but in some individuals it may manifest as abdominal discomfort or burping.
Beyond the gastrointestinal system, other side effects are less common. Injection site reactions (such as mild redness or itching at the injection site) can occur, but these are usually minor and self-limited. Allergic reactions are rare; however, if a patient experiences symptoms of anaphylaxis (e.g., widespread rash, swelling, trouble breathing) after an injection, they should seek emergency care and discontinue the medication. Hypoglycemia (low blood sugar) is not typically seen with tirzepatide on its own because it only triggers insulin release in the presence of elevated glucose. However, when tirzepatide is used in combination with other antidiabetic drugs (especially insulin or sulfonylureas), blood sugar levels can drop too low. Patients in such cases need to monitor glucose closely and may require dose adjustments of the concomitant diabetes medication to prevent hypoglycemia. Signs of low blood sugar (dizziness, shakiness, sweating, confusion) should be addressed promptly (with a fast-acting carbohydrate) and reported to the prescribing provider.[7]
Rare but serious adverse events associated with tirzepatide (and similar GLP-1 agonists) include pancreatitis and gallbladder issues. Acute pancreatitis has been reported infrequently; patients are advised to discontinue the medication and seek medical attention if they develop severe, persistent abdominal pain (especially if radiating to the back) with or without vomiting. Gallbladder problems such as cholelithiasis (gallstones) or cholecystitis have been observed in some individuals losing weight rapidly on incretin therapies. Maintaining adequate hydration and a slow, steady weight loss may mitigate this risk, but providers will monitor for symptoms like right-upper-quadrant pain. Another consideration is diabetic retinopathy: in patients with long-standing diabetes, a rapid improvement in blood glucose (and HbA1c) can sometimes transiently worsen retinopathy lesions . Thus, any changes in vision should be promptly evaluated by an ophthalmologist. Finally, although rodent studies showed thyroid C-cell tumors with tirzepatide, no cases of medullary thyroid carcinoma have been causally linked to GLP-1/GIP agonists in humans so far; nonetheless, any new neck mass, hoarseness, or difficulty swallowing should be evaluated to rule out thyroid pathology as a precaution.[7]
In summary, gastrointestinal side effects (nausea, vomiting, diarrhea, reduced appetite) are the most common with tirzepatide/niacinamide, especially during dose escalation⁷. These effects are usually manageable and tend to diminish over time. Other side effects may include injection site reactions, occasional headache or fatigue, and potential low blood sugar if combined with other diabetes medications. Patients should be educated on what to expect and advised to maintain communication with their healthcare provider. Most adverse effects can be mitigated by dose adjustments or supportive care (e.g., anti-nausea remedies, staying hydrated). The majority of patients do not experience severe side effects and find that the therapeutic benefits on blood sugar and weight outweigh the initial discomfort. However, it is crucial to use this medication under medical supervision so that any serious side effects (though rare) can be promptly identified and addressed.
Use in pregnancy is not recommended due to insufficient data and potential risks. Tirzepatide/niacinamide injection has not been studied in pregnant women, and its safety for the fetus is unknown. Given that poorly controlled diabetes in pregnancy is itself associated with adverse outcomes, it is important to manage blood glucose in pregnancy – but the preferred agents are insulin or certain oral medications with established safety records, rather than new agents like tirzepatide. Animal reproductive studies with tirzepatide have raised some concerns: high doses in pregnant rats and rabbits have been associated with developmental abnormalities (such as skeletal variations) and embryo-fetal loss . These findings suggest that tirzepatide exposure may pose risks to a developing fetus, including potential birth defects or miscarriage. Therefore, healthcare providers generally advise against using tirzepatide during pregnancy, and if a patient on tirzepatide becomes pregnant, the medication should be discontinued unless the potential benefit clearly outweighs the potential risk to the fetus.
Women of childbearing potential who are using tirzepatide should employ effective contraception to prevent pregnancy while on therapy. As noted in the Interactions section, tirzepatide can reduce the effectiveness of oral contraceptive pills, so a reliable barrier method or non-oral contraception is recommended to avoid an unplanned pregnancy.[1] If a patient is planning to conceive, it’s prudent to stop tirzepatide well in advance. Current guidance (for similar GLP-1 agonists) is to discontinue the medication at least 1–2 months before attempting pregnancy, to allow for the drug to be cleared from the body (tirzepatide has a long half-life of ~5 days, meaning it can persist for several weeks after the last dose). This washout period may help minimize any residual drug effects on early pregnancy.
For niacinamide, being a form of vitamin B3, normal dietary levels are essential in pregnancy, but the small additional amount in this injection is not known to confer any particular benefit or risk beyond standard prenatal vitamins. It is mainly the tirzepatide component that raises concern. In summary, tirzepatide/niacinamide injection should only be used during pregnancy if the potential benefit justifies the potential risk to the fetus. In practice, it is usually avoided in pregnant patients. Women taking this medication should have a clear discussion with their healthcare provider about effective contraception and the plan for glycemic control if they become pregnant or intend to become pregnant. If pregnancy occurs while on tirzepatide, the provider will likely discontinue the therapy and switch to an alternative diabetes treatment.[1]
With regard to breastfeeding, there is also limited information. It is not known whether tirzepatide is excreted in human breast milk. However, tirzepatide is a large peptide molecule (molecular weight ~4814 Da), so if any enters breast milk, the amounts would likely be very low and it would probably be destroyed in the infant’s digestive tract (making absorption by the baby unlikely).[8] Despite this, due to the lack of clinical data, caution is advised when considering tirzepatide in a nursing mother. Particularly for newborn or preterm infants, who might have more sensitive systems, it is generally recommended to avoid exposing them to tirzepatide via breast milk.[8] Niacinamide, by contrast, is a normal component of breast milk as a vitamin; the small dose in this injection would not be expected to pose harm to a breastfeeding infant. Even so, until more research is available, the conservative approach is to avoid tirzepatide/niacinamide while breastfeeding, or to use it only if the expected benefit to the mother is deemed to outweigh any potential risk to the infant. Mothers and healthcare providers should weigh the importance of maternal weight loss or diabetes control against the unknown effects on the breastfed child. In cases where postpartum glycemic control is needed, insulin or other medications with established lactation safety may be preferred. If tirzepatide is discontinued for breastfeeding, it can be reconsidered once the infant is weaned. Overall, decisions on pregnancy and lactation should be individualized and made in close consultation with a healthcare professional.[8]
Proper storage of tirzepatide/niacinamide injection is important to maintain its stability and potency. Upon receiving the medication, it should be stored in a refrigerator at 36°F to 46°F (2°C to 8°C). Keep the vials refrigerated when not in use, and do not allow them to freeze. If a vial does accidentally freeze, it should be discarded, as freezing can degrade the peptide. The medication can be kept at room temperature for short periods when preparing an injection, but prolonged exposure to room temperature should be avoided unless specified by the pharmacy.
Light exposure should be minimized, so it’s best to store the vials in their original carton or in an opaque container in the fridge. Keep all medications out of reach of children and pets, preferably in a designated medication area. Before each use, inspect the vial: the solution should be clear and colorless (or slightly pale yellow). If you notice particles, cloudiness, or discoloration, do not use that vial and contact the pharmacy for guidance.
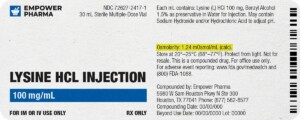
After puncturing the rubber stopper for the first dose, the vial becomes a multi-dose container. Use a new sterile needle and syringe for each withdrawal to maintain sterility. It is recommended to discard any unused portion 28 days after first puncture or by the beyond-use date (BUD) indicated on the label, whichever comes first. This 28-day rule helps ensure the medication remains effective and uncontaminated. Mark the date of first use on the vial as a reminder. Never “stretch” the use of a vial beyond the advised period.
When disposing of unused medication or expired vials, do not flush them down the toilet or pour them into drains. Instead, follow local guidelines for medication disposal – many pharmacies have take-back programs or specific instructions for safe disposal of injectables. Used needles and syringes should be placed in a FDA-cleared sharps disposal container (puncture-proof) rather than in household trash, to prevent needle-stick injuries.
In summary, store tirzepatide/niacinamide in the refrigerator, protect it from light and freezing, and observe the 28-day use window after opening. Proper storage and disposal not only ensure the medication’s effectiveness but also safety for those in the household.
- Farzam, K., & Patel, P. (2024). Tirzepatide. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK585056/
- Dahl, D., Onishi, Y., Norwood, P., Huh, R., Bray, R., Patel, H., … Rodríguez, Á. (2022). Effect of subcutaneous tirzepatide versus placebo added to titrated insulin glargine on glycaemic control in patients with type 2 diabetes: The SURPASS‑5 trial. JAMA, 327(6), 534–545. https://pmc.ncbi.nlm.nih.gov/articles/PMC8826179/
- Jastreboff, A. M., Aronne, L. J., Ahmad, N. N., Wharton, S., Connery, L., Alves, B., … Kaplan, L. M. (2022). Tirzepatide once weekly for the treatment of obesity (SURMOUNT‑1). The New England Journal of Medicine, 387(3), 205–216. https://doi.org/10.1056/NEJMoa2206038
- National Institutes of Health, Office of Dietary Supplements. (2023, July 7). Niacin: Fact sheet for health professionals. https://ods.od.nih.gov/factsheets/Niacin-HealthProfessional/
- National Library of Medicine. (n.d.). Niacin. In MedlinePlus Medical Encyclopedia. https://medlineplus.gov/ency/article/002409.htm
- Méndez‑Lara, K. A., Rodríguez‑Millán, E., Sebastián, D., Hernández‑Álvarez, M. I., Vicient, C. M., Herrero, L., & Zorzano, A. (2021). Nicotinamide protects against diet‑induced body‑weight gain, increases energy expenditure, and induces white adipose tissue beiging. Molecular Nutrition & Food Research, 65(11), e2100111. https://doi.org/10.1002/mnfr.202100111
- Meng, Z., Yang, M., Wen, H., Chen, J., & Zheng, J. (2023). A systematic review of the safety of tirzepatide—a new dual GLP‑1 and GIP agonist: Is its safety profile acceptable? Frontiers in Endocrinology, 14, 1121387. https://doi.org/10.3389/fendo.2023.1121387
- National Library of Medicine. (2023). Tirzepatide. In Drugs and Lactation Database (LactMed). https://www.ncbi.nlm.nih.gov/books/NBK581488/
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.
We're licensed to ship nationwide.
We ship orders directly to you, quickly and discreetly.




 Sermorelin Acetate ODT
Sermorelin Acetate ODT Ondansetron ODT
Ondansetron ODT Testosterone Cypionate / Testosterone Propionate Injection
Testosterone Cypionate / Testosterone Propionate Injection Semaglutide / Cyanocobalamin Injection
Semaglutide / Cyanocobalamin Injection Norditropin Injection
Norditropin Injection Tirzepatide ODT
Tirzepatide ODT Metformin Tablets
Metformin Tablets Zomacton Injection
Zomacton Injection Metformin Synergy Capsules
Metformin Synergy Capsules Omnitrope Injection
Omnitrope Injection